Chronic care management services
Overview of Chronic Care Management (CCM)
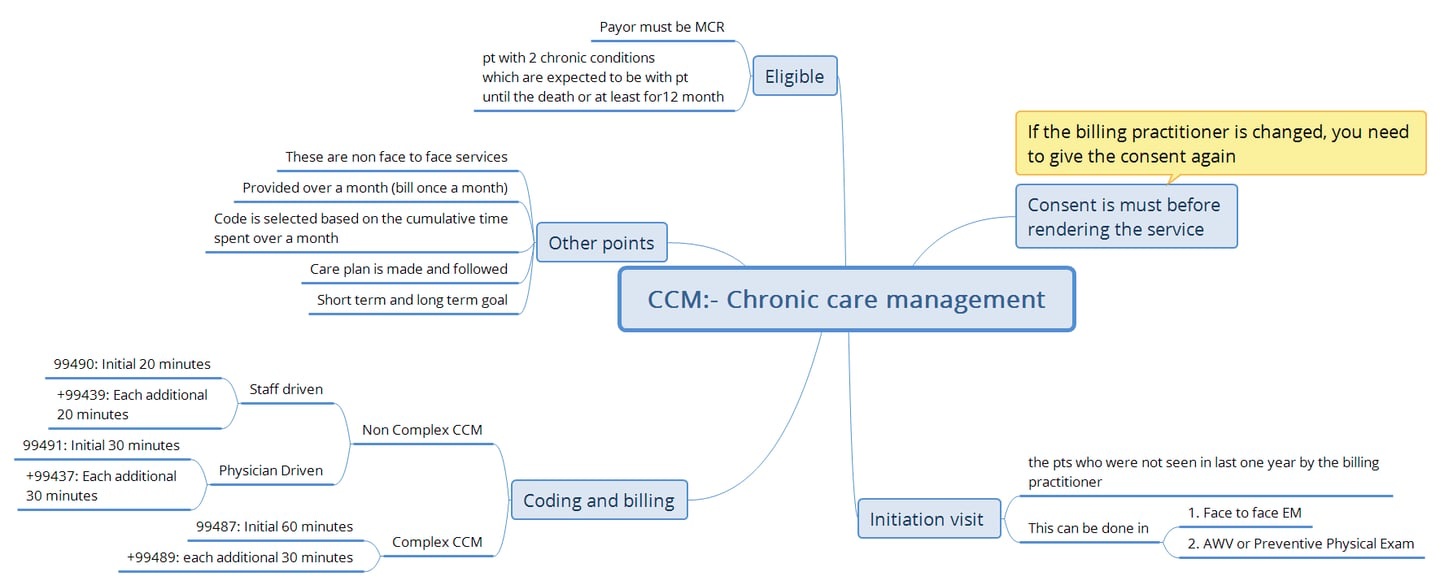
Chronic Care Management (CCM) is a crucial service recognized by the Centers for Medicare & Medicaid Services (CMS) that aims to improve health outcomes for Medicare patients with multiple chronic conditions. CCM services are designed to provide comprehensive care coordination and management outside of face-to-face visits, focusing on patients with two or more chronic conditions expected to last at least 12 months.
Key Elements of CCM Services
Patient Eligibility:
Patients must have multiple chronic conditions that are expected to last at least 12 months or until death.
Conditions must place the patient at significant risk of death, acute exacerbation, or functional decline.
Before CCM services can start, it is required an initiating visit for new patients or patients who you haven’t seen within the previous 1 year. Conduct the initiating visit during a comprehensive face-to-face E/M visit, annual wellness visit, or initial preventive physical exam.
Service Components:
Structured recording of patient health information.
Maintaining comprehensive electronic care plans.
Managing care transitions and coordinating care.
Providing 24/7 access to care and health information.
Practitioners Who Can Bill for CCM:
Certified Nurse Midwives (CNMs)
Clinical Nurse Specialists (CNSs)
Nurse Practitioners (NPs)
Physician Assistants (PAs)
Supervision:
CCM services can be provided under general supervision, meaning the billing practitioner does not need to be physically present.
Patient Consent:
Written or verbal consent must be obtained before billing for CCM services. Documentation of consent and patient information must be maintained in the medical record.
Comprehensive Care Plan:
A person-centered electronic care plan should be created, revised, and monitored, including problem lists, treatment goals, and medication management.
Billing Codes for CCM
CPT Codes:
99490: First 20 minutes of clinical staff time directed by a physician or qualified health care professional per calendar month.
99491: First 30 minutes provided personally by a physician or qualified health care professional per calendar month.
99487: Complex CCM services, first 60 minutes of clinical staff time.
99489: Each additional 30 minutes of complex CCM services.
99439: Each additional 20 minutes of clinical staff time.
99437: Each additional 30 minutes by a physician or qualified health care professional.
New Codes for Chronic Pain Management:
G3002: Monthly bundle for chronic pain management, including a required initial face-to-face visit.
G3003: Each additional 15 minutes of chronic pain management.
Important Billing Guidelines
Only one practitioner can bill for CCM services in a calendar month.
CCM services cannot be billed concurrently with certain other services (e.g., home health care supervision).
Time spent by clinical staff can count toward the billing threshold if directed by the billing practitioner.
RHCs and FQHCs can bill for CCM and Transitional Care Management (TCM) services for the same patient during the same period.
Common FAQs for CCM Coding and Billing
Can CCM services be delegated to clinical staff?
No, while clinical staff can assist, the billing practitioner must retain involvement in the CCM process.
What happens if a patient declines CCM services?
If a patient does not provide consent or declines services, the practitioner cannot bill for CCM.
Can CCM services be provided by practitioners outside the U.S.?
No, CCM services cannot be billed if provided by individuals located outside the United States.
Is a new patient consent required each month?
No, consent is required only once unless the patient switches billing practitioners.
What elements are required in the comprehensive care plan?
The care plan typically includes a problem list, expected outcomes, measurable treatment goals, and coordination with outside resources.