IP OP and consultation codes
Consultation
A consultation visit in medical coding is when a doctor (PCP) request specialist for his expert opinion or advice on a patient’s condition. Consultation is only considered when it is requested by the provider and not when patient goes himself to the specialist.
For example, if a primary doctor isn’t sure about the best way to treat a heart problem, they might request a cardiologist to evaluate the patient. The cardiologist would then perform a consultation visit to provide their expert advice.
Consultation
To bill the consultation, 3R are required.
R: Request by the PCP, this is also recognized as referring physician
R: Rendering, Consulting physician render (provide) the service
R: Report back, consulting physician send report back to the PCP with thank you note.
If any R is missing, then consultation cannot be coded.
Outpatient Consultation
An outpatient consultation happens when a patient visits a doctor or specialist for a second opinion or expert advice about a specific health issue on request of PCP. This type of visit usually happens outside of a hospital setting, like in a clinic or doctor’s office.
(Note: If patient goes by himself to another specialist without request of PCP, then this visit for second opinion will NOT be considered as consultation, it will be coded as new patient to the specialist if seen first time)
Here’s a simple breakdown of the process:
Referral: The patient's primary doctor (referred to as the referring provider) suspects a specific issue and refers the patient to a specialist for expert advice or a detailed evaluation. For example, if a patient has ongoing chest pain, the primary doctor might refer them to a cardiologist.
Consultation Visit: The patient sees the specialist (referred to as the consulting provider). The specialist reviews the patient’s history, performs any necessary examinations or tests, and then discusses their findings with the patient.
Report Back: After the consultation, the specialist sends a report to the referring provider. This report includes the findings, recommendations for treatment, and any follow-up advice
Consultation can be billed only once. Subsequent visit with the consulting physician in outpatient is billed with office established patient codes (99212 to 99215. Outpatient consultation is coded with following codes:
Consultation coding for Medicare Payor:
Medicare has stopped paying the consultation code from 2010. To solve this, physician would be billed with cross walked code. For Outpatient, it is coded with new pt code.
Scenario
Example 1 (Non-Medicare): A cardiologist is requested by a primary care physician to provide their expert opinion on a patient’s heart condition. The cardiologist spends 45 minutes with the patient, discussing their condition and providing advice and reporting back to PCP with thank you note. In this case, the cardiologist would bill using the outpatient consultation code 99244 (Based on the time).
Example 2 (Medicare): A similar scenario as above, but the patient is a Medicare beneficiary. The cardiologist would bill using the appropriate E/M code instead of the consultation code and here it would be billed with 99204.
Scenario :- Outpatient Consultation
Primary Care Physician’s Request: A 60-year-old woman undergoes a routine check-up, and her ECG shows irregularities. Concerned about possible cardiac issues, the PCP refers the patient to a cardiologist for further evaluation and management of suspected arrhythmia.
Consulting Provider's Action: The cardiologist conducts a thorough assessment, reviews the patient’s medical history, and performs additional tests, including an echocardiogram. The cardiologist determines that the patient has atrial fibrillation and recommends initiating medication to control the rhythm. A detailed consultation report is sent to the PCP, outlining the findings and the treatment plan.
Consultation is billed only per specialty:
A consultation is only billed once for each specialist. If the patient needs to see the same specialist again later, those follow-up visits are not considered consultations anymore. Instead, they are billed as regular visits for established patients, meaning the doctor already knows the patient.
Scenario:
First Visit (Consultation):
A primary care doctor refers a patient with chest pain to a cardiologist. The cardiologist sees the patient for the first time, reviews the patient's condition, performs tests, and sends a report back to the primary doctor. This visit is billed as a consultation.
Follow-Up Visits (Established Patient):
The patient comes back to the cardiologist for follow-up care, like reviewing test results or adjusting medications. These visits are no longer consultations because the cardiologist already knows the patient. Instead, these follow-up visits are billed under established patient codes.
This rule applies to outpatient consultations—after the first consultation, all further visits with the same specialist are coded differently.
Inpatient Consultation
Inpatient Consultation:
An inpatient consultation is when a specialist is asked to evaluate a patient who has been admitted to a hospital. Just like with outpatient consultations, the specialist is brought in by the patient’s primary doctor (or attending physician) to give their expert opinion on a specific issue or condition while the patient is hospitalized.
Key Points of Inpatient Consultation:
Request: The primary doctor or another healthcare provider at the hospital requests the consultation. This could be due to a new or ongoing medical problem that requires a specialist’s evaluation or advice.
Consultation Visit: The consulting physician (specialist) visits the patient in the hospital, reviews the medical history, examines the patient, and might order tests or procedures. Based on this, the specialist gives their recommendations or treatment plan.
Report Back: The specialist sends a detailed report back to the primary or attending doctor. This report includes the findings, advice, and next steps.
If any R is missing, then it can be coded with subsequent visit code
Example:
A 68-year-old patient is admitted to the hospital with pneumonia. During the stay, the attending physician observes the patient experiencing increased shortness of breath and wheezing, raising concerns about a potential COPD exacerbation. The attending physician requests a pulmonologist to consult.
Consultation Visit: The pulmonologist visits the patient, evaluates the respiratory status, reviews the medical history, and orders a chest X-ray. The pulmonologist diagnoses a COPD exacerbation secondary to pneumonia and recommends initiating bronchodilator therapy, starting antibiotics, and adjusting the patient's oxygen supplementation.
Report Back: The pulmonologist writes a report detailing the diagnosis and treatment recommendations, which is sent to the attending physician, who continues managing the patient’s pneumonia alongside the pulmonology interventions
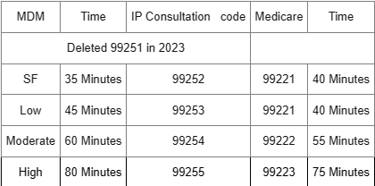
9925199252: Inpatient or observation consultation for a new or established patient, which requires a medically appropriate history and/or examination and straightforward medical decision making. When using total time on the date of the encounter for code selection, 35 minutes must be met or exceeded.
99253: Inpatient or observation consultation for a new or established patient, which requires a medically appropriate history and/or examination and low level of medical decision making. When using total time on the date of the encounter for code selection, 45 minutes must be met or exceeded.
99254: Inpatient or observation consultation for a new or established patient, which requires a medically appropriate history and/or examination and moderate level of medical decision making. When using total time on the date of the encounter for code selection, 60 minutes must be met or exceeded.
99255: Inpatient or observation consultation for a new or established patient, which requires a medically appropriate history and/or examination and high level of medical decision making. When using total time on the date of the encounter for code selection, 80 minutes must be met or exceeded.
Consultation coding for Medicare Payor:
Medicare has stopped paying the consultation code from 2010. To solve this, coder has to cross to hospital/observation codes.
Initial consultation is cross walked to initial hospital/observation code (99221 to 99223).
Subsequent consultation for same specialty for during that continuous length of stay is coded with subsequent hospital/observation codes (99231 to 99233).
Consultation coding for hospital/observation code: - Consultation can be billed once per specialty per length of stay. subsequent consultation is coded for same specialty for same length of stay is coded with subsequent hospital/observation care codes (99231 to 99233).
Inpatient - Hospital care codes
Hospital or observation care codes are divided based on the initial visit, subsequent visit, and discharge visit.