Critical Care
Critical care means that a doctor or a skilled healthcare provider is giving urgent medical attention to a very sick or seriously injured patient, where if the critical care is not provided then the patient may further deterioration of the condition.
To bill the critical care following are requirements:
Critical condition(s)
Aggressive Intervention
Time excluding other billable procedures (minimum 30 minutes is required to bill the critical care)
A critical illness or injury severely affects one or more important organ systems, putting the patient at high risk of immediate, life-threatening deterioration.
Conditions that could call for critical care include (but are not limited to):
Central nervous system failure
Circulatory failure
Shock
Renal hepatic, metabolic and/or respiratory failure
Overwhelming infection
Tips:
Medicare rules state that only one doctor can report critical care for a patient on a single day, even if multiple doctors are involved in the patient's care. Any other doctors who provided care should use the subsequent hospital care codes (99231-99233) instead of critical care codes.
Let's say a doctor in the emergency room is taking care of a patient in shock. After 25 minutes, the patient becomes more stable and is no longer in immediate life-threatening danger.
In this situation, since the critical care lasted less than 30 minutes, you should use a regular emergency room visit code, not the special 99291 code for critical care.
The time a doctor spends on critical care doesn't have to be all at once; it can be in separate parts. You just add up all the time spent on critical care for a specific date to get the total.
For example, if the doctor provides one hour of critical care to stabilize the patient, and then later on the same day, the patient's condition gets worse, and the doctor spends another hour, you can use code 99291 for the first hour and code 99292 (which means two additional hours) for the second hour, even though they weren't continuous.
When critical care extends past midnight, CPT rules say to bill the total time as one service if it's continuous. If there's a break, a new service starts and you can bill 99291 again.
Bundle procedure into Critical care:
For healthcare professionals reporting critical care services, the following services are considered part of critical care when performed by the physician(s) during the critical care period:
Interpretation of cardiac output measurements (93598).
Interpretation of chest X-rays (71045, 71046).
Pulse oximetry monitoring and interpretation (94760, 94761, 94762).
Analysis of blood gases.
Collection and interpretation of physiologic data, such as ECGs (electrocardiograms), blood pressure readings, and hematologic data.
Gastric intubation procedures (43752, 43753).
Temporary transcutaneous pacing (92953).
Ventilatory management, including services identified by codes 94002, 94003, 94004, 94660, and 94662.
Vascular access procedures, which are covered by codes 36000, 36410, 36415, 36591, and 36600.
Any other services performed during critical care that are not listed above should be reported separately. Healthcare facilities may also report these services separately if necessary.
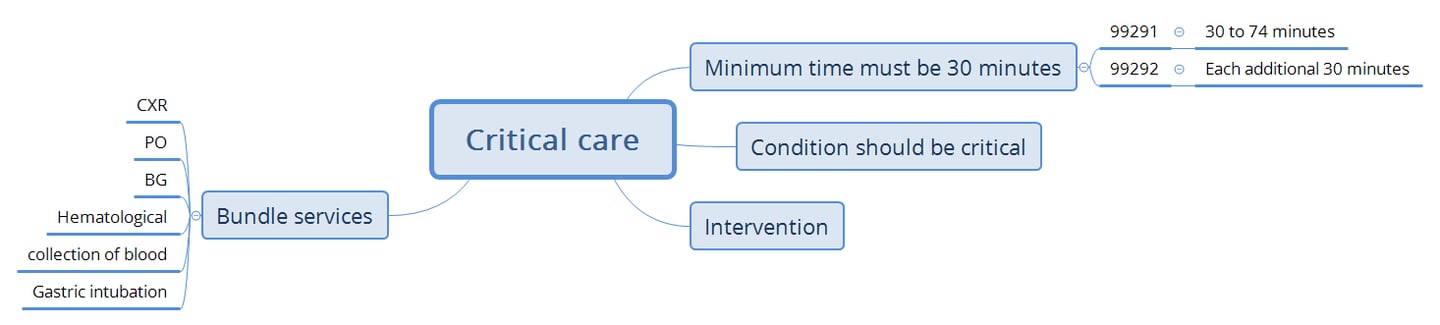
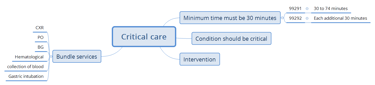
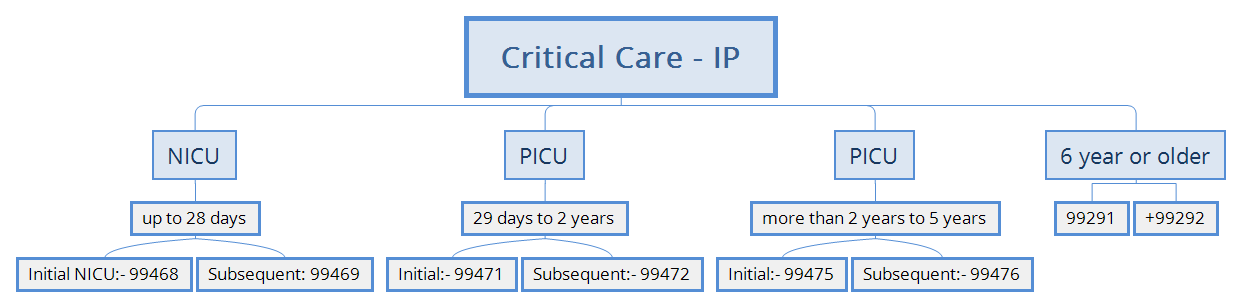
Time:
The doctor has to spend at least 30 minutes excluding other billable procedures giving important medical care to a patient for it to be considered critical care, as per the rules. If the care takes less than 30 minutes, the doctor will use a different code for the visit, following the guidelines.
Aggressive Intervention:
Critical care involves making complex decisions to evaluate, control, and support these vital systems, either to treat a single or multiple organ failure or to prevent further life-threatening deterioration. Critical care often involves monitoring various physiological indicators and using advanced technologies, it can also be given in emergency situations where these tools aren't available. Critical care may continue over multiple days, even if the treatment doesn't change, as long as the patient's condition still demands the same level of attention.
Critical Care and Other Same-Day Evaluation and Management (E/M) Visits:
When critical care services are reported the same date as another E/M visit, the medical record documentation must support:
1) that the other E/M visit was provided prior to the critical care services at a time when the patient did not require critical care,
2) that the services were medically necessary, and
3) that the services were separate and distinct, with no duplicative elements from the critical care services provided later on that date.
Scenario 1:
When an E/M visit is performed in the morning and critical care is provided later in the evening, both services can be billed.
This is because the E/M visit occurred before the patient required critical care, the services are medically necessary, and they are separate and distinct with no duplicative elements.
Use modifier -25 on the E/M claim to indicate it is a significant, separately identifiable service from the critical care.
Scenario 2:
When critical care is provided in the morning and an E/M visit is performed later in the evening, only the critical care services should be billed.
This is because the patient was already under critical care in the morning, and any subsequent E/M visit on the same day is considered part of the critical care services and not separately billable.
In this scenario, billing for both services is not allowed due to the overlapping nature of the care provided.
Critical Care - Practice report 1
Patient Name: John Evans
MRN: 98745621
Date of Admission: 09/29/2024
Date of Critical Care: 09/29/2024
Attending Physician: Dr. Sarah Lewis
Primary Diagnosis: Acute respiratory failure due to COVID-19 pneumonia
Secondary Diagnosis: Acute kidney injury
Hospital Course:
John Evans, a 62-year-old male, was admitted with acute hypoxemic respiratory failure secondary to severe COVID-19 pneumonia. His oxygen saturation dropped below 85%, and he developed tachypnea and increased work of breathing. He was immediately intubated and placed on mechanical ventilation. Initial settings included high levels of positive end-expiratory pressure (PEEP) and FiO2 of 100%. Despite these interventions, Mr. Evans experienced persistent hypoxemia and required prone positioning to improve oxygenation. Continuous monitoring of arterial blood gases and ventilator settings was performed, along with sedation and paralytics to facilitate oxygenation. Total time spent during the critical care service was 135 minutes.
Key Interventions:
Intubation and mechanical ventilation: needed 5 minutes to perform.
Prone positioning for ARDS
Arterial blood gas monitoring
Sedation and paralytics
Discharge Condition:
Remains critical, sedated and ventilated. Close monitoring of ventilator settings and arterial blood gases continues.
Critical Care - Practice report 2
Patient Name: Maria Gonzalez
MRN: 54621387
Date of Admission: 09/26/2024
Date of Critical Care: 09/27/2024
Attending Physician: Dr. Thomas Monroe
Primary Diagnosis: Septic shock secondary to urosepsis
Secondary Diagnoses: Acute kidney injury, Metabolic acidosis
Hospital Course:
Maria Gonzalez, a 75-year-old female, presented with fever, confusion, and hypotension. Blood cultures revealed Escherichia coli (E. coli) urosepsis. She developed septic shock with multi-organ failure, requiring immediate vasopressor support with norepinephrine to maintain a mean arterial pressure (MAP) of 65 mmHg. A central venous catheter was placed for vasopressor administration and fluid resuscitation. The patient was also started on continuous renal replacement therapy (CRRT) due to acute kidney injury with metabolic acidosis. Time was spent adjusting vasopressor dosages and fluids, monitoring vital signs, and managing metabolic derangements. Total time spent during the critical care was 160 minutes.
Key Interventions:
Central venous catheter placement
Vasopressor support with norepinephrine
Continuous renal replacement therapy (CRRT)
Discharge Condition:
Critical, with continued need for CRRT and vasopressors. Transferred to ICU for ongoing care.
Critical Care - Practice report 3
Patient Name: David Simmons
MRN: 87654213
Date of Admission: 09/25/2024
Date of Critical Care: 09/26/2024
Attending Physician: Dr. Lisa Miller
Primary Diagnosis: Traumatic brain injury with subdural hematoma
Secondary Diagnoses: Increased intracranial pressure (ICP), Hypotension
Critical Care Time: 145 minutes
Hospital Course:
David Simmons, a 27-year-old male, sustained a traumatic brain injury following a motor vehicle accident. He arrived at the hospital unconscious with a Glasgow Coma Scale (GCS) of 4. A CT scan revealed a large subdural hematoma with signs of increased intracranial pressure (ICP). The patient was intubated and hypertonic saline was administered to reduce ICP. An intracranial pressure monitor was placed, and close monitoring of ICP and hemodynamic parameters was performed. The patient experienced episodes of hypotension, requiring vasopressors to maintain cerebral perfusion. Frequent adjustments of sedation, vasopressors, and fluids were necessary to prevent further neurological damage.
Key Interventions:
Intracranial pressure (ICP) monitoring
Hypertonic saline administration
Vasopressor support for hypotension
Discharge Condition:
Condition remains critical, with ongoing need for ICP monitoring and vasopressor therapy. Transferred to neurosurgical ICU for further management.
Critical Care - Practice report 4
Patient Name: Richard Williams
MRN: 54721365
Date of Admission: 09/23/2024
Date of Critical Care: 09/24/2024
Attending Physician: Dr. James Harris
Primary Diagnosis: Cardiogenic shock following acute myocardial infarction
Secondary Diagnoses: Pulmonary edema, Acute renal failure
Critical Care Time: 180 minutes
Hospital Course:
Richard Williams, a 68-year-old male, presented with an acute anterior myocardial infarction. He developed cardiogenic shock with pulmonary edema and worsening renal function. An emergency percutaneous coronary intervention (PCI) was performed, placing two drug-eluting stents in the left anterior descending (LAD) artery. Post-PCI, Mr. Williams required inotropic support with dobutamine and norepinephrine to maintain adequate cardiac output and blood pressure. Diuresis was initiated with intravenous furosemide to manage pulmonary edema. Continuous hemodynamic monitoring and frequent adjustments of inotropic medications were required to stabilize his condition.
Key Interventions:
Percutaneous coronary intervention (PCI) with stent placement
Inotropic support with dobutamine and norepinephrine
Diuresis for pulmonary edema management
Discharge Condition:
Stable but critical, requiring continued inotropic support. Transferred to cardiac ICU for further management.
Critical Care - Practice report 5
Patient Name: Amanda Clark
MRN: 43125786
Date of Admission: 09/22/2024
Date of Critical Care: 09/22/2024
Attending Physician: Dr. Samuel White
Primary Diagnosis: Anaphylactic shock following bee sting
Secondary Diagnosis: Hypotension, Respiratory distress
Critical Care Time: 110 minutes.
Hospital Course:
Amanda Clark, a 42-year-old female, was brought to the emergency department after a bee sting triggered an anaphylactic reaction. She experienced hypotension, angioedema, and severe respiratory distress. Epinephrine was administered intramuscularly, followed by intravenous fluids and antihistamines. Despite initial treatment, Ms. Clark developed persistent hypotension and required intravenous epinephrine infusion. She was intubated due to progressive airway swelling and respiratory failure. Continuous hemodynamic monitoring and epinephrine titration were performed over the next 110 minutes until her condition stabilized.
Key Interventions:
Epinephrine administration (IM and IV)
Intubation for airway protection
Intravenous fluid resuscitation
Discharge Condition:
Condition stabilized after epinephrine and fluids, remains intubated. Transferred to ICU for continued care.