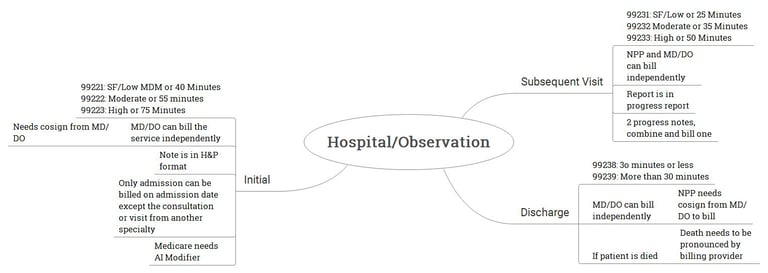
Inpatient - Hospital care or Observation Care
Inpatient coding: refers to the process of assigning codes to medical procedures, diagnoses, and services provided to patients who are admitted to a hospital or other healthcare facility for an overnight stay or longer. Inpatient coding is primarily used for reimbursement purposes, as it helps healthcare providers accurately bill insurance companies and government payers for the services rendered.
Hospital or observation care are divided in
Initial Hospital or observation care
Subsequent Hospital or observation care
Discharge from Hospital or observation care
Date: December 31, 2023
Morning - Admission: Mr. Sharma, a 65-year-old male, is admitted to the hospital with severe chest pain. The attending physician, Dr. Patel, evaluates him and suspects a heart condition. Dr. Patel documents an admission note detailing Mr. Sharma’s symptoms, medical history, and initial treatment plan. This admission note is then billed.
Evening - Progress Note: Dr. Patel visits Mr. Sharma again in the evening to assess his condition. He notes that Mr. Sharma’s chest pain has lessened due to the medication. Dr. Patel documents a progress note outlining the patient’s response to treatment and any changes made to the treatment plan. However, only the admission note from the morning is billed for this day.
Date: January 2, 2024 - Discharge: on January 2, 2024, Dr. Patel sees Mr. Sharma in the morning and makes a progress note. However, this progress note is not billed separately. Later in the evening, when Dr. Patel discharges Mr. Sharma, a discharge note is prepared and billed. So, for this day, only the discharge visit is coded and billed. This is in line with the usual practice where only the most significant visit (in this case, the discharge) is billed on any given day.
AI Modifier:
AI modifier is appended to H&P note done for admission purpose when the payor is Medicare.
The AI modifier is used to identify the principal physician of record during an inpatient admission. This modifier should only be used by the admitting or attending physician overseeing the patient’s care during a hospital or nursing facility admission.
This modifier can be appended with 99221 to 99223, 99304 to 99306, and critical care code when critical care was warranted at the time of admission.
Admission notes: an Admission Note, also known as an H&P (History and Physical) note, is a crucial part of a patient’s medical record. It documents the patient’s status, including their history and physical examination findings, the reasons why the patient is being admitted for inpatient care to a hospital or other facility, and the initial instructions for that patient’s care.
MD or DO can perform the admission independently and get billed.
NPPs can not perform the admission independently, they need cosign from the MD/DO
Subsequent Note (Progress Note): Progress notes are clinical notes made by healthcare professionals involved in a patient’s treatment and care. They contain clinical facts and medical reasoning about the care delivered to patients and the clinical events relevant to diagnosis and treatment. They are professional documents that communicate important information on a patient’s condition between multiple providers.
Progress note can be documented by NPP alone as well. No cosign from MD/DO are needed.
Discharge Note: A discharge note, also known as a termination, note or discharge summary, is a written summary held in the client’s chart of what happened during the time the client was in your care. It is often the primary mode of communication between the hospital care team and aftercare providers. It includes reasons for termination, symptoms at the time of intake, initial reasons for seeking treatment, diagnosis, treatment goals, modalities and interventions used, progress made during treatment, and recommendations for future mental health care needs.
Discharge can be billed independently by MD/DO. NPPs needs cosign by MD/DO.
Admission Reports
Admission Note 1:
Date: 2024-07-04
Admitting Physician: Dr. John Doe, MD
Chief Complaint: Chest pain
HPI:
The patient is a 65-year-old male presenting with a 2-hour history of substernal chest pain radiating to the left arm. The pain is described as severe and crushing, associated with diaphoresis and nausea. The patient denies any previous history of similar symptoms.
ROS: Cardiovascular: Positive for chest pain. Respiratory: No dyspnea, no cough. Gastrointestinal: Nausea present, no vomiting.
Neurological: No headaches, no dizziness.
PFSH: Past Medical History: Hypertension, hyperlipidemia. Family History: Father had a myocardial infarction at age 70. Social History: Smoker, 1 pack per day for 40 years, occasional alcohol use.
Physical Examination:
Vital Signs: BP 150/90, HR 90, RR 18, Temp 98.6°F. Cardiovascular: S1, S2 normal, no murmurs, rubs, or gallops. Respiratory: Clear to auscultation bilaterally. Abdomen: Soft, non-tender, no hepatosplenomegaly. Neurological: Alert and oriented, cranial nerves intact.
MDM:
EKG shows ST elevation in the anterior leads.
Troponin levels elevated.
Diagnosis: Acute myocardial infarction.
Plan:
Admit to the coronary care unit (CCU).
Start aspirin, clopidogrel, and heparin.
Consult cardiology for urgent catheterization.
Admission Note 2:
Date: 2024-07-04
Admitting Physician: Dr. Jane Smith, DO
Chief Complaint: Shortness of breath
HPI:
The patient is a 75-year-old female presenting with progressive shortness of breath over the past week. The patient reports orthopnea and paroxysmal nocturnal dyspnea. She denies any recent chest pain or fever.
ROS:
Cardiovascular: No chest pain, orthopnea present.
Respiratory: Shortness of breath, no cough.
Gastrointestinal: No nausea or vomiting.
Neurological: No dizziness or weakness.
PFSH:
Past Medical History: Congestive heart failure, atrial fibrillation.
Family History: Mother had chronic heart disease.
Social History: Non-smoker, no alcohol use.
Physical Examination:
Vital Signs: BP 140/80, HR 100, RR 22, Temp 98.4°F.
Cardiovascular: Irregular rhythm, S3 present.
Respiratory: Bibasilar crackles.
Abdomen: Soft, non-tender.
Extremities: 2+ pitting edema in lower extremities.
MDM:
Chest X-ray shows pulmonary congestion.
BNP levels elevated.
Diagnosis: Acute exacerbation of congestive heart failure.
Plan:
Admit to telemetry.
Start diuretics and oxygen therapy.
Monitor fluid status and electrolytes.
Admission Note 3:
Date: 2024-07-04
Admitting Physician: Dr. Alex Turner, MD
Chief Complaint: Abdominal pain
HPI:
The patient is a 50-year-old male with a 1-day history of severe abdominal pain localized to the right lower quadrant. The pain is constant and aggravated by movement. The patient reports associated nausea and anorexia.
ROS:
Gastrointestinal: Abdominal pain, nausea, no vomiting.
Cardiovascular: No chest pain, no palpitations.
Respiratory: No cough, no dyspnea.
Neurological: No dizziness, no headaches.
PFSH:
Past Medical History: Appendectomy, hypertension.
Family History: No relevant family history.
Social History: Non-smoker, occasional alcohol use.
Physical Examination:
Vital Signs: BP 130/85, HR 85, RR 18, Temp 99.1°F.
Abdomen: Tenderness in the right lower quadrant, rebound tenderness present.
Cardiovascular: S1, S2 normal.
Respiratory: Clear to auscultation bilaterally.
MDM:
Abdominal ultrasound suggests acute cholecystitis.
WBC count elevated.
Diagnosis: Acute cholecystitis.
Plan:
Admit to general surgery.
Start IV antibiotics.
Prepare for laparoscopic cholecystectomy.
Admission Note 4:
Date: 2024-07-04
Admitting Physician: Dr. Emily Johnson, DO
Chief Complaint: Fever and confusion
HPI:
The patient is an 80-year-old female presenting with a 2-day history of fever and confusion. The patient has been disoriented and unable to perform daily activities. There is no history of recent travel or sick contacts.
ROS:
General: Fever present.
Neurological: Confusion, no focal deficits.
Cardiovascular: No chest pain, no palpitations.
Respiratory: No cough, no shortness of breath.
PFSH:
Past Medical History: Type 2 diabetes, hypertension.
Family History: No relevant family history.
Social History: Lives alone, non-smoker, no alcohol use.
Physical Examination:
Vital Signs: BP 110/70, HR 90, RR 20, Temp 101.2°F.
Neurological: Disoriented to time and place, no focal neurological deficits.
Cardiovascular: S1, S2 normal.
Respiratory: Clear to auscultation bilaterally.
Abdomen: Soft, non-tender.
MDM:
Blood cultures pending.
Urinalysis suggests urinary tract infection.
Diagnosis: Urosepsis.
Plan:
Admit to medical ward.
Start broad-spectrum antibiotics.
Monitor vitals and mental status.
Admission Note 5:
Date: 2024-07-04
Admitting Physician: Dr. Michael Lee, MD
Chief Complaint: Severe headache
HPI:
The patient is a 45-year-old female presenting with a sudden onset of severe headache described as "the worst headache of her life." The pain is diffuse and associated with photophobia and nausea. The patient has no history of similar headaches.
ROS:
Neurological: Severe headache, photophobia.
Cardiovascular: No chest pain, no palpitations.
Respiratory: No cough, no dyspnea.
Gastrointestinal: Nausea present, no vomiting.
PFSH:
Past Medical History: Migraine headaches.
Family History: No relevant family history.
Social History: Non-smoker, no alcohol use.
Physical Examination:
Vital Signs: BP 145/95, HR 95, RR 18, Temp 98.6°F.
Neurological: Alert, oriented, photophobia present, no focal deficits.
Cardiovascular: S1, S2 normal.
Respiratory: Clear to auscultation bilaterally.
MDM:
CT scan of the head shows subarachnoid hemorrhage.
Lumbar puncture confirms elevated opening pressure.
Diagnosis: Subarachnoid hemorrhage.
Plan:
Admit to neurology intensive care unit (NICU).
Start nimodipine.
Consult neurosurgery.
Discharge Notes
Discharge Note 1
Patient Name: Sarah Williams
MRN: 54321876
Date of Admission: 09/20/2024
Date of Discharge: 09/25/2024
Attending Physician: Dr. Amanda Chen
Primary Diagnosis: Acute uncomplicated pyelonephritis
Secondary Diagnosis: None
Hospital Course:
Sarah Williams, a 32-year-old female, was admitted with fever and flank pain. Urinalysis revealed pyuria, and urine culture confirmed E. coli infection. She was treated with intravenous ceftriaxone, showing improvement by day 2, with resolution of fever and reduction in pain.
Final Physical Exam:
Vitals: BP 118/76, HR 78, Temp 98.2°F
Heart: Regular rate and rhythm
Lungs: Clear to auscultation
Abdomen: Non-tender, no rebound tenderness
Discharge Medications:
Ciprofloxacin 500 mg orally twice daily for 5 days
Ibuprofen 400 mg as needed for pain
Discharge Instructions:
Complete the course of antibiotics
Maintain hydration (at least 8 glasses of water daily)
Return to hospital if fever or pain worsens
Follow-Up:
Primary care follow-up in one week
Discharge Condition:
Stable, afebrile, tolerating oral fluids.
Discharge Time: 25 minutes
Disposition: Discharged home in stable condition.
Discharge Note 2
Patient Name: George Thompson
MRN: 87654312
Date of Admission: 09/14/2024
Date of Discharge: 09/21/2024
Attending Physician: Dr. John Peterson
Primary Diagnosis: Acute decompensated heart failure
Secondary Diagnosis: Hypertension, Hyperlipidemia
Hospital Course:
George Thompson, a 70-year-old male with a history of chronic heart failure, was admitted for worsening dyspnea and edema. He was treated with intravenous diuretics, resulting in symptom improvement. Time was spent educating the patient and family on medication adherence, fluid restriction, and weight monitoring.
Final Physical Exam:
Vitals: BP 130/82, HR 70, O2 Sat 97% on room air
Heart: Regular rate, S3 present
Lungs: Clear
Extremities: 1+ edema bilaterally
Discharge Medications:
Furosemide 40 mg daily
Spironolactone 25 mg daily
Metoprolol 50 mg twice daily
Discharge Instructions:
Limit daily fluid intake to 1.5 liters
Low-sodium diet (less than 2g/day)
Daily weight monitoring; report weight gain of more than 3 pounds in 24 hours
Take medications as prescribed
Follow-Up:
Follow-up with cardiology in 5 days
Home health services arranged
Discharge Condition:
Stable with mild residual edema.
Discharge Time: 45 minutes
Disposition: Discharged home with family support.
Discharge Note 3: Surgical Discharge
Patient Name: Emily Davis
MRN: 43219876
Date of Admission: 09/18/2024
Date of Discharge: 09/21/2024
Attending Surgeon: Dr. Melissa Brown
Primary Diagnosis: Status post-laparoscopic appendectomy (99490 - post op period is 90 days)
Secondary Diagnosis: None
Hospital Course:
Emily Davis underwent successful laparoscopic appendectomy following a diagnosis of acute appendicitis. She recovered well post-operatively, resuming oral intake and ambulation by day 2. Surgery was performed on 9/19/2024.
Final Physical Exam:
Vitals: BP 112/70, HR 75
Abdomen: Soft, non-tender, laparoscopic incisions healing well
Discharge Medications:
Acetaminophen 500 mg as needed for pain
Ondansetron 4 mg as needed for nausea
Discharge Instructions:
Avoid heavy lifting for 4 weeks
Monitor for signs of infection at incision sites
Follow up with surgeon in 2 weeks
Discharge Condition:
Stable, healing well post-operatively.
Discharge Time: 20 minutes
Disposition: Discharged home in good condition.
Discharge Note 4: Discharge to Skilled Nursing Facility
Patient Name: Betty Green
MRN: 56743219
Date of Admission: 09/10/2024
Date of Discharge: 09/24/2024
Attending Physician: Dr. Richard Hall
Primary Diagnosis: Ischemic stroke with left-sided weakness
Secondary Diagnosis: Hypertension, Type 2 Diabetes
Hospital Course:
Betty Green was admitted with acute ischemic stroke. She received thrombolytic therapy and recovered gradually. Although her condition improved, she continues to have significant left-sided weakness and requires rehabilitation.
Final Physical Exam:
Vitals: BP 145/90, HR 68
Neuro: Left-sided weakness (3/5 strength)
Discharge Medications:
Aspirin 81 mg daily
Amlodipine 5 mg daily
Metformin 1000 mg twice daily
Discharge Instructions:
Participate in physical therapy at the SNF
Monitor blood sugar and blood pressure daily
Report any worsening of neurological symptoms
Follow-Up:
Neurology follow-up in 2 weeks
Physical therapy at SNF
Discharge Condition:
Stable, requiring assistance for mobility.
Discharge Time: 50 minutes
Disposition: Transferred to SNF for rehabilitation.
Discharge Note 5: Discharge to Skilled Nursing Facility
Patient Name: Michael Brown
MRN: 19876543
Date of Admission: 09/08/2024
Date of Discharge: 09/17/2024
Attending Physician: Dr. Lisa Carter
Primary Diagnosis: Diabetic ketoacidosis (DKA)
Secondary Diagnosis: Type 1 Diabetes Mellitus
Hospital Course:
Michael Brown was admitted in diabetic ketoacidosis. He required IV insulin therapy and careful electrolyte management in the ICU. After stabilization, he was transitioned to subcutaneous insulin. Extensive education was provided on insulin administration and glucose monitoring.
Final Physical Exam:
Vitals: BP 125/78, HR 80, Glucose controlled
Endocrine: No signs of ketoacidosis
Discharge Medications:
Insulin glargine 20 units at bedtime
Insulin lispro before meals
Discharge Instructions:
Check blood glucose before meals and at bedtime
Administer insulin as prescribed
Attend diabetes education sessions
Follow-Up:
Endocrinology follow-up in 7 days
Appointment for diabetes education
Discharge Condition:
Stable with blood sugar control.
Discharge Time: 60 minutes
Disposition: Discharged home.