Table B: Amount and/or Complexity of Data to Be Reviewed and Analyzed
The "amount and/or complexity of data to be reviewed and analyzed" refers to how much and how complicated the information is that healthcare providers need to look at during a patient visit. This includes things like medical records, test results, and other information that helps them make decisions about the patient's care.
The complexity of the data can change based on things like how many tests or documents they need to review, where the information is coming from, and if they need to talk to other healthcare providers or outside sources.
Straight forward (None) and Low Complexity data (minimal)
Some points to consider in ordering and reviewing:
In medical coding, ordering a test is considered part of the test result category, and reviewing the test results is part of the overall encounter. It's assumed that a physician or other qualified healthcare professional (QHP) will review the results of any test they order. Because of this, it's generally best practice to give credit for ordering the test rather than for reviewing it. In other words, you can give credit for either ordering or reviewing the test, but not both, when determining the level of medical decision making (MDM) for the service.
Please note that providers of the same specialty, are considered a single physician. This is confirmed in the CPT Assistant FAQ.
Question: If I order a CT scan at a visit on June 10 and review it with the patient at a follow-up visit on June 17, would I count the order on the 10th and the review on the 17th? This applies even if I did not bill for the CT scan or its interpretation.
Answer: No, count only once.
What is mean by unique test?
A unique test is defined by the CPT code set but when a doctor compares multiple results of the same unique test (like checking blood sugar levels several times), it is counted as just one unique test, even if there are multiple results for example, If a doctor orders blood glucose tests at different times throughout the day to compare the result, these multiple results are considered part of one unique test, even if repeated.
Also, tests that have parts that overlap with each other are not considered unique, even if they have different codes.
For example,
85025: A Complete Blood Count (CBC) with automated differential includes various components, such as hemoglobin (Hgb), hematocrit (Hct), red blood cell count (RBC), white blood cell count (WBC), and platelet count. Even though some of these components have individual CPT codes, they are not considered unique tests in the context of Medical Decision Making (MDM) because they share overlapping elements. The automated differential WBC count is also included within this test, meaning that all these elements together count as one unique test.
Here is the list of individual components within a Complete Blood Count (CBC) with differential (CPT code 85025) and their respective CPT codes when ordered individually:
Hemoglobin (Hb) - CPT Code 85018
Hematocrit (Hct) - CPT Code 85014
Red Blood Cell Count (RBC) - CPT Code 85041
White Blood Cell Count (WBC) - CPT Code 85048
Platelet Count - CPT Code 85049
Automated Differential WBC Count - CPT Code 85025 (as part of CBC with differential, but 85027 for CBC without differential)
When these components are ordered together as part of a CBC with differential (85025), they are counted as one unique test in Medical Decision Making (MDM) since they are grouped under a single CPT code.
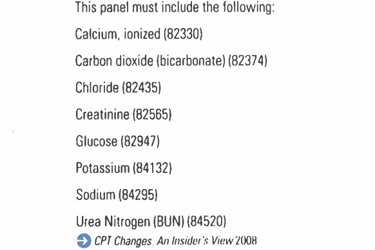
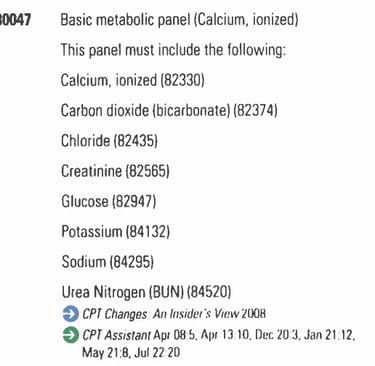
Let's say a provider orders an electrolyte panel (CPT code 80051), which includes four individual tests: carbon dioxide (bicarbonate) (CPT code 82374), chloride (CPT code 82435), potassium (CPT code 84132), and sodium (CPT code 84295). Despite including multiple tests, the electrolyte panel is considered one unique test, not four.
On the other hand, tests that have overlapping elements are not considered unique, even if they have distinct CPT codes. For example, a CBC with differential and a CBC without differential would be considered one unique test because they have overlapping components.

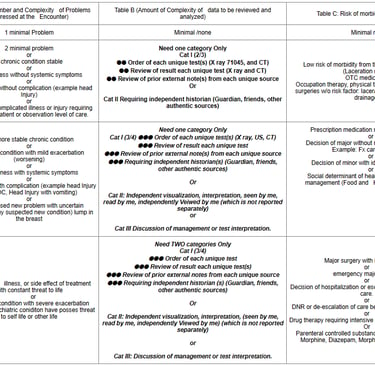
Moderate Data Complexity
Not separately reported
If a test or study is independently seen by physician and finding has been drawn by himself, and it's not billed separately, then it's considered part of the decision-making process.
However, if the doctor bills for a separate CPT code specifically for interpreting the test or study, that interpretation doesn't count as part of the decision-making process for the visit.
Example 1:
If a physician performs an E/M service and interprets an EKG, documenting three findings out of the seven to eight possible, the interpretation, and minimum three points, lead to billing the CPT code 93010 (professional component).
However, since the interpretation is used to bill for the 93010 code, it is not considered determining the level of medical decision making (MDM) for the E/M service.
EKG Coding
TO bill the EKG, following 2 points must be met.
Interpretation done by the provider. Statement or similar verbiage must be documented.
Each billable EKG should have at 3 points from the following: -
Rate
Rhythm
Comparison with prior EKG
PR wave Interval
ST segment change
QRS complex
Summary of clinical Condition
Example 2:
Question: In a cardiology practice, if my cardiology partner completes the official echo report and bills for it, but I later see the patient and interpret the echo, can I consider this an independent interpretation?
Answer: No, you cannot. If your cardiology partner, who is also in the same specialty as you, reported the professional component and billed for it, you should not credit an independent interpretation when you see the patient. But yes, you can consider the interpretation in MDM when another group of physicians had interpreted the echo.