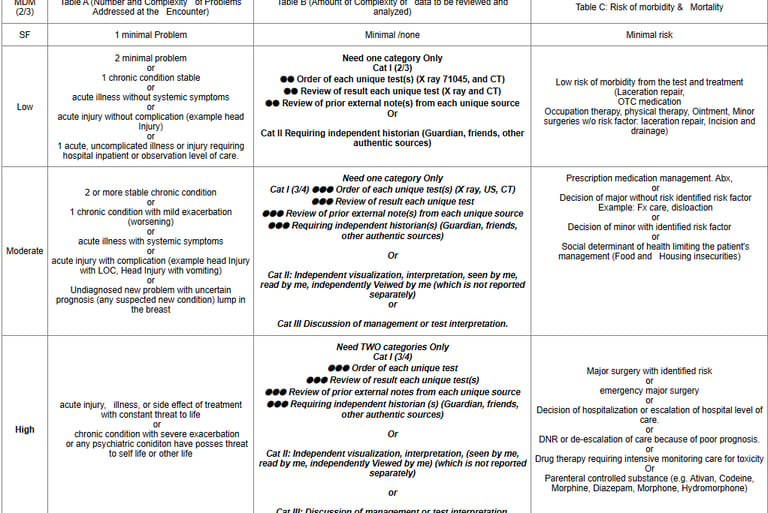
Table C: Risk of Complications and/or Morbidity or Mortality of Patient Management
The risk of complications and/or morbidity or mortality of patient management refers to the likelihood and potential consequences of adverse events associated with decisions made during a medical encounter regarding diagnostic procedures and treatments.
Please note that it is the risk arising from procedure or diagnostic test not from the disease condition itself. Risk from disease condition itself it decides the COPA while risk with test and procedure decides the table C.
Table A (COPA) focuses on the risk from the condition itself.
Risk Table focuses on the risk from the diagnosis and management of the condition.
Minimal and Low risk of Morbidity from additional Diagnostic or treatment

Surgeries (Minor or Major, elective, emergency procedure or patient risk):
Surgery - Minor or Major: - The classification of surgery into minor or major is based on the common meaning of such terms when used by trained clinicians, similar to the use of the term “risk.” These terms are not defined by a surgical package classification.
Surgery - Elective or Emergency: Elective procedures and emergent or urgent procedures describe the timing of a procedure when the timing is related to the patient’s condition. An elective procedure is typically planned in advance (eg, scheduled for weeks later), while an emergent procedure is typically performed immediately or with minimal delay to allow for patient stabilization. Both elective and emergent procedures may be minor or major procedures.
Surgery - Risk Factors, Patient or Procedure: Risk factors are those that are relevant to the patient and procedure. Evidence-based risk calculators may be used, but are not required, in assessing patient and procedure risk.
Moderate risk of Morbidity from additional Diagnostic or treatment
Prescription drug management:
We are easily giving the credit for when physician is prescribing the new medication, also we give the credit when dosage being adjusted, both increasing or decreasing, but we become little uneasy when the visit is for prescription refill.
It's crucial to understand that even during a visit for a prescription refill, the physician considers the patient's interval status, which includes reviewing the patient's medical record for any relevant information. This may also involve reviewing the results of any tests that were previously decided to be done at this encounter.
Also, other thought is that by looking at the risk table definition, the definition says the risk of mortality and morbidity associated with diagnostic testing and treatment and refilling the medication is nothing but allowing patient to take the medication, and it is the medication which is one is associated with risk. Hence prescription refill will also be considered for moderate risk. However, it is essential to document the drug name and dosage for accurate coding. Without this information, it is unclear which medication is being refilled and at what dosage. Remember, the thumb rule of medical coding is "if not documented, not done!" This emphasizes the importance of thorough documentation to accurately reflect the services provided.
Also, it is NOT when physician simply write "continue with current medication" without specifying the drug and dosage. However, it's important to note that credit can be given for prescription drug management in this scenario, but only if the physician explicitly specifies the medication and dosage.
When a physician writes "continue with current medication [X] [dosage]," it demonstrates active management of the patient's medication regimen. This documentation shows that the physician is making a conscious decision to continue the current medication, taking into account the patient's health status and interval history. It also indicates that the physician has reviewed the patient's medical record and considered any relevant information, such as test results or changes in the patient's condition.
This level of detail is crucial for accurately coding prescription refill visits. Without specifying the medication and dosage, it's difficult to determine the complexity of the decision-making process involved. This can lead to undercoding, which can have financial implications for healthcare providers and impact the accuracy of patient records.
In conclusion, while it may seem trivial, documenting prescription refills with specificity regarding the medication and dosage is essential for accurate E/M coding. It ensures that the complexity of the decision-making process is appropriately reflected, leading to more accurate coding and better patient care.
Social Determinants of health:
These are the non-medical factors like where you live, work, and play, which can have a profound impact on your health. Let's explore these game-changers:
1. Income and Social Protection:
- Income: Money talks, especially in health. Higher incomes often mean better access to healthcare and a healthier lifestyle.
- Social Protection: Think of it as a safety net. Things like social insurance and unemployment benefits can make a big difference in your overall health.
2. Education:
- The more you know, the healthier you might be. Education can lead to better decision-making, job opportunities, and healthier habits.
3. Unemployment and Job Insecurity:
- Unemployment: Losing a job can lead to stress and health issues due to financial strain.
- Job Insecurity: Even the fear of losing a job can impact mental health and overall well-being.
4. Working Life Conditions:
- Your work environment matters. Stressful or unsafe conditions can take a toll on your health.
5. Food Insecurity:
- Not having enough nutritious food can lead to health problems like malnutrition and chronic diseases.
6. Housing, Basic Amenities, and the Environment:
- Your home is your health haven. Safe and stable housing is crucial for your well-being.
7. Early Childhood Development:
- What happens early in life can affect your health later on. Access to good nutrition and education in childhood can set the stage for a healthy future.
These factors can either level the playing field or tilt it, leading to health inequities. Surprisingly, they can have a bigger impact (30-55%) on health outcomes than healthcare itself! Addressing these social determinants requires a united effort across different sectors. It's not just about treating illnesses; it's about creating a healthier world for everyone.
Drug therapy requiring intensive monitoring for toxicity:
When a drug has potential side effects that could lead to serious harm or even death, it often needs intensive monitoring. This type of monitoring is mainly done to catch possible adverse effects, not necessarily to check how well the drug is working. Here’s a straightforward breakdown of what intensive monitoring involves, along with some examples to make it clearer.
Purpose: The primary goal is to detect side effects or potential harms, not the drug’s effectiveness.
Method of monitoring: Monitoring may be performed by Lab method, Radio method or by physiologic test, monitoring of toxicity by history and physical is not acceptable.
Timing: Intensive monitoring can be short-term (such as during the initial stages of treatment) or long-term (over the months or years the patient takes the drug). Long-term monitoring typically occurs at least every three months.
Common Toxicity effects:
What is Cytopenia? Cytopenia refers to a decrease in one or more types of blood cells (red blood cells, white blood cells, or platelets). This condition can result from various causes, including bone marrow suppression due to chemotherapy.
Consequences of Cytopenia:
Increased Risk of Infection: A low white blood cell count (leukopenia) makes patients more susceptible to infections. Symptoms might include fever, chills, or other signs of infection, which can become life-threatening if not promptly addressed.
Bleeding and Bruising: A low platelet count (thrombocytopenia) increases the risk of bleeding. Patients may experience easy bruising, prolonged bleeding from cuts, or spontaneous bleeding (e.g., nosebleeds).
Fatigue and Weakness: A low red blood cell count (anemia) can lead to symptoms like fatigue, weakness, and shortness of breath, significantly impacting the patient's quality of life.
Monitoring Strategies:
To prevent and manage cytopenia effectively, healthcare providers may implement the following monitoring strategies:
Frequent Complete Blood Count (CBC): Regular blood tests to monitor the levels of different blood cells, allowing for early detection of cytopenia.
Adjusting Chemotherapy Regimens: If cytopenia is detected, providers may reduce the dosage or delay treatment cycles to allow the bone marrow to recover.
Utilizing Growth Factors: In some cases, medications such as granulocyte colony-stimulating factor (G-CSF) can be administered to stimulate the production of white blood cells.